SWISS Heroin Assisted Treatment 1994 – 2025: SUMMARY
SWISS HAT (Heroin Assisted Treatment) APPROACH TO opioid ADDICTION
1994 – 2025: SUMMARY
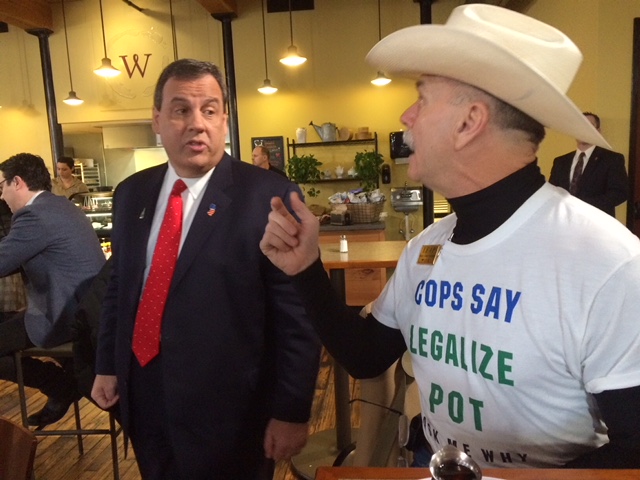
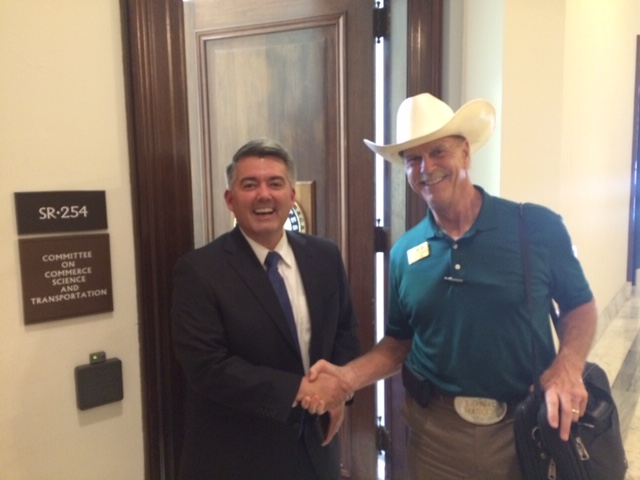
This summary was taken from six published reports and updated every year. The Swiss Federal Office of Public Health reviewed and approved its release for 2021. Additional questions should be directed to Dr. Anna Rickley in Bern (41) 58-469-18-13 Email Anna.Rickley@bag.admin.ch Dr. Rickley is native fluent in German, and fluent inEnglish. NOTE: The author toured Swiss clinics in 2001, 2008 & 2016 and met with federal health officials in September 2022 and 7 other occasions to increase understanding and knowledge. Understanding was enhanced, due to the author’s fluency in French and German. This summary was researched and written by Howard J. Wooldridge, Drug Policy Specialist at Citizens Opposing Prohibition (.org)
Overview: Due to the severe drug problem in Switzerland in the early 1990s, (rising number of injection drug users, visibility of open drug scenes, AIDS epidemic, rising number of drug related deaths, poor physical health, high criminality) the Swiss made a fundamental shift in approaching the problems caused by heroin addiction. The Swiss offer treatment-on-demand and life-time status as a patient. (Like an alcoholic is a lifelong condition) A variety of different treatments is available, in order to treat a broad range of dependent people. Of an estimated 22-24,000 addicted people 17,500 are in treatment. 92% are given daily doses of primarily methadone (orally) at conventional clinics or via general practitioners (60%). The Swiss treat about 1600 dependent people with maintenance doses of heroin (diacetylmorphine) or slow-release morphine tablets at 23 special clinics operating in cities and two prisons. Opioid based treatments are part of a broader therapy that includes social, educational and psychological measures. The Swiss approach has resulted in lower rates of crime, death, disease, a slight drop in expected new users as well as an improvement in mental and physical health, employment and housing. Similar programs have been developed in eight other countries: Germany, Portugal, Denmark, Holland, Belgium, England, Spain and Canada.
The Swiss HAT program is covered by health insurance.
* To qualify for a treatment with dia-morphine: 1) at least 18 years old; 2) been severely dependent ; 3) present signs of poor health; 4) two or more failed attempts of conventional treatment (methadone or other) 5) dia-morphine can only be obtained at the clinic and must be taken on site (oral or injection). (Note: Under strict control and specific criteria a few are allowed to take away one oral dose daily). During Covid, this rule has been further relaxed.
A. Patients can receive up to three doses of dia-morphine per day. 66% take it via needle injection, the rest orally.
B. Patients average about three (3) years in this plan. However, they may stay in treatment indefinitely. 20% of original patients are still in the program.
C. Upon relapse, a patient can return to the clinic and re-start the treatment.
D. The vast majority of patients are satisfied or very satisfied with the program.
E. Average age of patient: 59 years.
F. The Swiss approach is custom-designed, according to the medical needs of the patient.
*Crime Issues: 60% drop in felony crimes by patients (80% drop after one year in the program). 82% drop in patients selling heroin.
*Death Rates: Millions of doses have been administered. No participant has died from a heroin overdose since the inception of the program.
*Disease Rates: New infections of Hepatitis and HIV have been reduced for patients.
*New Use Rates: Slightly lower than expected. 1) As reported in the Lancet June 3, 2006, the medicalization of using heroin has tarnished the image of heroin and made it less attractive to young people. This is still true in 2025 per Bern. 2) Most new users are introduced to heroin by members of their social group and 50% of users also deal to support their habit. Therefore, with so many users/sellers in treatment, non-users have fewer opportunities to be exposed to heroin, especially in the rural areas.
*Cost Issues: 50 dollars/day: Patient costs are covered by national health insurance agency. Patients pay annually 700 dollars for the compulsory insurance. Note: The Swiss save about 40 dollars per day per patient mostly in lowered costs for court and police time, due to less crime committed by the patients.
*The Swiss annually purchase about 250 kilos of heroin for treatment. Since 1994 Swiss patients have received over 20,000,000 doses of heroin without a fatality.
** The Swiss approach gives us a glimpse of a context in which drug issues are handled by the medical community.
*** In October 2024, the Swiss govt health representatives in Bern confirmed their readiness to explain their program to the US Congress, if they receive a formal request.
**** The Swiss do not have an opioid-type problem like in the USA
Reader: What the Swiss Program is not:
A. It has not eliminated street sales of heroin. Dealers still exist in cities with clinics.
B. It is not a ‘free’ drugs program. Patients must purchase health care insurance and receive their methadone or heroin as part of their comprehensive therapy.
C. A non-heroin using adult cannot walk into a clinic and receive heroin.
D. Simply put; the Swiss are using a comprehensive, public health approach (treatment on demand) to heroin addiction whose unique feature is to allow a small minority of patients to receive pure, maintenance doses of heroin or morphine.
E. Heroin is not available for purchase in Switzerland.
Due to Covid, the Swiss have changed the procedures, so that patients can now take their Di-M home for a maximum of 7 days.